In our previous newsletters, we addressed the improvement of energy for AtremoPlus users. In this new edition, we will focus on a related theme: chronic fatigue and daytime sleepiness.
Feeling constantly tired and lacking energy, even to stay awake during the day, is extremely difficult to live with. Being alert and fully present is essential in daily life, yet chronic fatigue and daytime sleepiness make life considerably more difficult for individuals affected by Parkinson’s. For family members, especially life partners, it can also be burdensome to see the person often exhausted or even absent.
The results of our recent survey on this topic are particularly positive, and we are delighted that the groups most affected by daily or very frequent chronic fatigue and daytime drowsiness have experienced a decrease of 82.35%.
Many individuals have been able to move from “chronic fatigue” and “frequent daytime sleepiness” to a “more occasional” situation of these distressing phenomena. Furthermore, a significant number of people have left these two groups, with a more significant rebound, and no longer experience this phenomenon.
Only 11.75% have not experienced any improvement in terms of chronic fatigue and daytime sleepiness.
At AtremoPlus, we foster a culture of learning and nurture a deep desire to understand and convey the underlying mechanisms of action of active ingredients in various issues. According to the saying “knowledge is power,” at AtremoPlus, we might say “an informed client is MORE powerful”  .
.
In the first part of this newsletter, we will attempt to summarize all the physiological, neurological, and psychological/emotional factors inherent in chronic fatigue and daytime drowsiness in Parkinson’s disease.
Then, to delve deeper, we will further explore the fascinating field of brainwaves in the second part.
Beyond understanding the mechanisms, we will strive to take an additional indispensable step by rigorously measuring the results because without measurement, there is no science. The famous Italian mathematician Galileo, often considered the father of modern science, expressed the importance of measurement in science with this quote:
“Measure what is measurable, and make measurable what is not yet so.”
That is why the third part is dedicated to a study conducted in 2023, focusing on measuring brain activity, specifically brainwaves, before and after taking AtremoPlus.
Part 1 – Chronic Fatigue and Daytime Sleepiness in Parkinson’s Disease
Chronic fatigue and daytime sleepiness in Parkinson’s disease have multiple origins and stem from a very complex mix of interactions. However, we can synthesize some of the most important ones:
1. Dopamine Deficiency:
Parkinson’s disease leads to a decrease in dopamine production, a key neurotransmitter for controlling movement and energy. This deficit causes a general feeling of fatigue and a reduction in available energy.
2. Mitochondrial Dysfunction:
Individuals with Parkinson’s disease often have mitochondrial abnormalities, as mitochondria are responsible for energy production. Inefficient energy production at the cellular level can lead to chronic fatigue. (See link to our latest newsletter issue 17 on this subject below).
3. Sleep Disorders:
People with Parkinson’s often suffer from sleep disorders such as insomnia, restless leg syndrome, and involuntary movements during the night. More recently, researchers have also discovered that restless nights with nightmares are common and may even be a precursor to Parkinson’s disease. Disrupted sleep contributes to increased daytime fatigue and drowsiness. (See our newsletters 2, 3, 4 on this topic).
4. Medication Side Effects:
Treatments for Parkinson’s disease, such as chemical L-Dopa, can cause side effects, including daytime drowsiness and fatigue. Fluctuations in medication levels can also affect sleep-wake cycles. If you have any questions about this, we recommend discussing them with your doctor.
5. Depression, Stress, and Anxiety:
These disorders are common in people with Parkinson’s and can intensify feelings of fatigue and drowsiness. Depression, in particular, is associated with a loss of energy and increased drowsiness.
6. Increased Physical Effort:
Due to muscle stiffness and slow movements, people with Parkinson’s often have to exert more effort to perform daily activities, which can exhaust them more quickly.
7. Autonomic Issues:
Parkinson’s disease can affect the autonomic nervous system, responsible for regulating many bodily functions, including sleep-wake cycles. Dysfunctions in this system can lead to excessive daytime sleepiness.
2 – The Fascinating Universe of Brain Waves
In our recent newsletter on energy, we delved into the mechanisms of cellular energy production as well as broader systems such as organs and muscles, particularly focusing on biochemical aspects. This time, we will dive deeper into the electrical aspect of functioning because, without being fully aware, many of our vital processes rely on electrical currents!
The headquarters of electrical commands reside in the brain.
The entire body is traversed by an extensive network of neurons that transmit electrical currents to regulate certain functions, such as muscle activation, heartbeats, or even respiration. These electrical currents play a fundamental role in regulating various mental and bodily states.
This neuronal network is particularly dense in the brain, where brain waves are electrical oscillations produced by the synchronized activity of neurons. Each region of the brain is responsible for certain functions, and the intensity of activity in these regions allows us to assess their degree of activation. This electrical activity is detectable through techniques such as electroencephalography (EEG). Brain waves vary in frequency and amplitude and are classified into five main types, ranging from the slowest to the fastest waves, each associated with different states of consciousness and mental activities.
1. Delta Waves (0.5 to 4 Hz): These low-frequency waves are predominant during deep dreamless sleep. They are crucial for body regeneration and repair.
2. Theta Waves (4 to 8 Hz): These waves are present during light sleep phases and deep meditation. They are also associated with creativity, intuition, and learning.
3. Alpha Waves (8 to 13 Hz): Alpha waves generally appear when the mind is calm and relaxed but present and not asleep.
4. Beta Waves (13 to 30 Hz): These waves are associated with an active wakeful state, concentration, and intensive cognitive processes. They predominate when we are engaged in highly active and awake mental activities.
5. Gamma Waves (30 to 100 Hz): Gamma waves are the fastest and are linked to high cognitive processes such as perception, consciousness, and complex problem-solving. They are also involved in coordinating different brain regions for information processing.
Brain waves play an essential role in regulating our mental and emotional states. They are influenced by various factors such as sleep, meditation, stress, and concentration.
Dysfunction of Brain Waves in Parkinson’s Disease
Over the years, researchers have found that brain waves, in the context of Parkinson’s disease, undergo alterations. These modifications may be linked to issues such as chronic fatigue and daytime sleepiness.
Although science is still far from being able to correlate all parameters, we can discern certain trends of dysfunction in these brain waves for individuals affected by Parkinson’s.
1. Delta Waves (0.5 to 4 Hz):
– Normal: Associated with deep sleep and regeneration.
– Parkinson’s: Individuals with Parkinson’s may exhibit disturbances in Delta waves, which can contribute to sleep disturbances and inadequate regeneration during the night, exacerbating chronic fatigue. It is common to observe the brain regularly entering Delta states during the day, plunging individuals into states of drowsiness.
2. Theta Waves (4 to 8 Hz):
– Normal: Associated with deep relaxation, dreams, and creativity.
– Parkinson’s: Theta waves may be altered, affecting sleep quality and increasing daytime sleepiness. Some individuals with Parkinson’s may appear absent-minded at times and may struggle to be fully present in the moment.
3. Alpha Waves (8 to 13 Hz):
– Normal: Associated with a state of relaxation and calm, yet present.
– Parkinson’s: A decrease in Alpha waves is often observed, leading to difficulties in achieving a relaxed state while being conscious and present, thus contributing to fatigue and drowsiness.
4. Beta Waves (13 to 30 Hz):
– Normal: Associated with active wakefulness, concentration, and cognitive processes.
– Parkinson’s: An abnormal increase in Beta waves may be observed, often associated with neuronal hyperactivity that may be linked to tremors and rigidity. This can also disrupt sleep-wake cycles, increasing fatigue. Several studies also suggest that Beta waves are present during sleep, accompanied by distressing dreams. Additionally, researchers even consider restless sleep over longer periods as a precursor to Parkinson’s disease.
5. Gamma Waves (30 to 100 Hz):
– Normal: Associated with high cognitive processes and neuronal coordination.
– Parkinson’s: Alterations in Gamma waves can disrupt cognitive functions and coordination, indirectly contributing to mental and physical fatigue. These very rapid waves may manifest during sleep as nighttime terrors, which is a significant issue in the context of Parkinson’s disease. It is worth noting that high stress, whether occasional or chronic, as well as experienced traumas, may contribute to the development of Parkinson’s disease. This intriguing topic will be further developed in one of our upcoming newsletters.
While brain waves are a complex subject requiring further research, it can be concluded that there is a disorder in these different waves in individuals with Parkinson’s disease.
Regarding chronic fatigue and daytime sleepiness, it is interesting to note that in some individuals with Parkinson’s, brain waves appear somewhat inverted. Indeed, some of these individuals exhibit very slow waves (Delta and Theta) during the day, often placing them close to the threshold of falling asleep. Conversely, for others, waves can be very fast at night, sometimes accompanied by distressing dreams, whether remembered or not.
If you regularly experience restless sleep, it may be helpful to discuss certain emotions, whether in a professional or private setting, to alleviate associated stress. It is true that we may not have learned to express our emotions and talk about our traumas of various kinds. Thus, our brains try to “resolve” these traumas at night in our dreams, which can become distressing over time.
3 – Study on the Improvement of Brain Waves in Different Stages of Parkinson’s Disease with Our Dietary Supplement
In our quest to quantify the elements of improvement, we wish to share with you the results of a study conducted on the evolution of brain waves before and after the intake of AtremoPlus.
The study was carried out with individuals at three different stages of Parkinson’s disease:
- Individuals with Parkinson’s without cognitive impairment
- Individuals with Parkinson’s disease with mild cognitive impairment
- Individuals with Parkinson’s disease with dementia
The results are particularly interesting because measurements of brain waves before taking AtremoPlus reveal a predominance of Delta and Theta waves, which are associated with slow brain activity characteristic of daytime sleepiness. However, after taking AtremoPlus, we clearly observe an increase in the frequency of brain waves towards Alpha waves during a measurement taken 1 hour after intake.
Below are two typical images of the electroencephalogram measurement before and one hour after taking AtremoPlus with a dose of 5g:
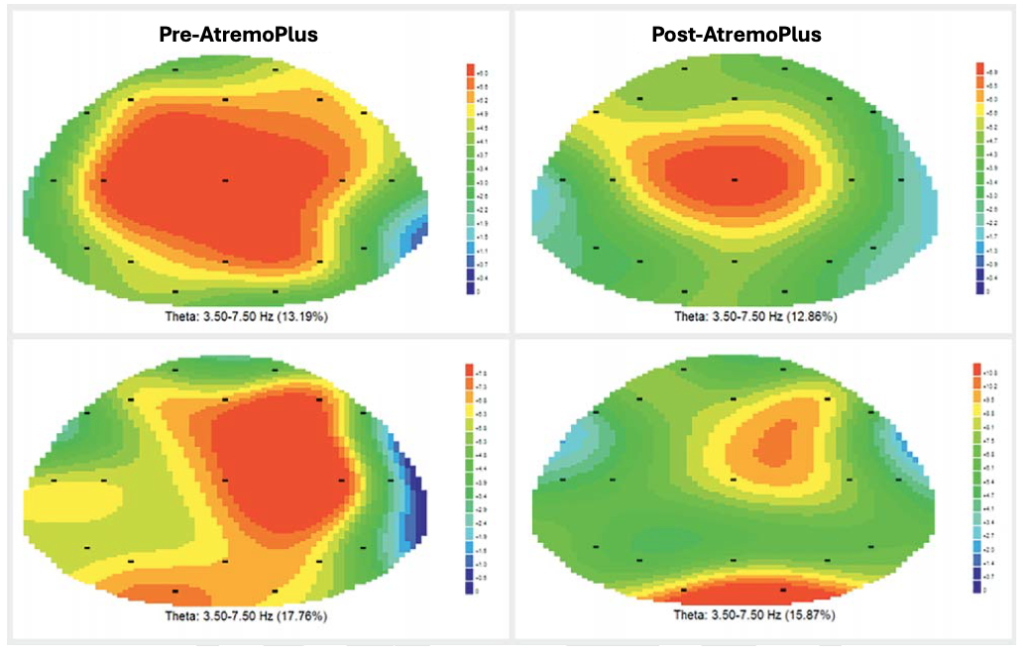
The red areas correspond to slow Theta waves, often associated with drowsiness, while the Alpha waves, represented in green, are faster. They indicate a state of relaxation while remaining awake and present.
Taking two doses of 5 g per day (equivalent to four daily sachets), as practiced by the majority of our clients, promotes twice a day an increase in fast Alpha waves oscillating in your brain, making you both more awake and relaxed, while reducing the very slow Delta and Theta waves, associated with drowsiness.
Your sensations translate into measurable and visible improvements, thanks to very effective monitoring.
In a quest for understanding, we enthusiastically welcome your positive individual feedback as well as the broader feedback on specific survey topics, to compare them with the data collected in studies on our dietary supplement.
To illustrate, in the case of chronic fatigue and daytime drowsiness, we can confidently assert that your improvement observations perfectly match the conclusions of our study on brain waves. This study indeed notes an increase in brain wave speed, resulting in greater presence and increased wakefulness after taking AtremoPlus.
Naturally, your individual feelings are paramount, as what matters most is perceiving an improvement in your attention and presence. However, it’s interesting to note that these sensations are not merely subjective, but can be corroborated and measured with improvements in biomarkers or, as seen here, with the observation of enhanced brain waves.
We will conclude this newsletter with Myriam’s testimony, which could well be linked to an improvement in her brain waves:
“Since I started taking AtremoPlus, I see the difference in my energy level when walking, and in the morning, I am immediately connected to reality, whereas if I don’t take it, I have a low gaze, my head feels like it’s in a vice, and I remain in a brain fog for a good part of the day.”
Furthermore, our next newsletter will continue to emphasize measurements, as combined with your feelings, they form a perfect alliance and mutually reinforce each other.
This content may be important for people who need this natural solution. Thanks for sharing !
By clicking on the button below, I leave the information site:
Disclaimer:
Please note that this blog provides information about our dietary supplement AtremoPlus and related topics.
This blog is not intended to provide medical advice.
If you have any medical questions, please contact your healthcare professional.
References :
He, Xuetao, et al. “The patterns of EEG changes in early-onset Parkinson’s disease patients.” International Journal of Neuroscience 127.11 (2017): 1028-1035.
Bhat, Shreya, et al. “Parkinson’s disease: Cause factors, measurable indicators, and early diagnosis.” Computers in biology and medicine 102 (2018): 234-241.
Shirahige, Livia, et al. “Quantitative electroencephalography characteristics for Parkinson’s disease: a systematic review.” Journal of Parkinson’s Disease 10.2 (2020): 455-470.
Stumpf, Kilian, et al. “Effects of Parkinson’s disease on brain-wave phase synchronisation and cross-modulation.” Europhysics Letters 89.4 (2010): 48001.
Bose, A. and Beal, M.F. (2016), Mitochondrial dysfunction in Parkinson’s disease. J. Neurochem., 139: 216-231
Winklhofer, Konstanze F., and Christian Haass. “Mitochondrial dysfunction in Parkinson’s disease.” Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease 1802.1 (2010): 29-44.
Exner, Nicole, et al. “Mitochondrial dysfunction in Parkinson’s disease: molecular mechanisms and pathophysiological consequences.” The EMBO journal 31.14 (2012): 3038-3062.
Abou-Sleiman, Patrick M., Miratul MK Muqit, and Nicholas W. Wood. “Expanding insights of mitochondrial dysfunction in Parkinson’s disease.” Nature Reviews Neuroscience 7.3 (2006): 207-219.
Latif, Saad, et al. “Dopamine in Parkinson’s disease.” Clinica chimica acta 522 (2021): 114-126.
Espay, Alberto J., Peter A. LeWitt, and Horacio Kaufmann. “Norepinephrine deficiency in Parkinson’s disease: the case for noradrenergic enhancement.” Movement Disorders 29.14 (2014): 1710-1719.
Sathya Prabhu, D., and V. Devi Rajeswari. “Nutritional and biological properties of Vicia faba L.: A perspective review.” International Food Research Journal 25.4 (2018): 1332-1340.
Dhull, Sanju Bala, et al. “A review of nutritional profile and processing of faba bean (Vicia faba L.).” Legume Science 4.3 (2022): e129.
Ryu, Jaihyunk, et al. “Fatty acid composition, isoflavone and L-3, 4-dihydroxyphenylalanine (L-dopa) contents in different parts of faba bean (Vicia faba) genotypes.” Plant breeding and Biotechnology 5.4 (2017): 314-324.
Kempster, P. A., and M. L. Wahlqvist. “Dietary factors in the management of Parkinson’s disease.” Nutrition reviews 52.2 (1994): 51.
Nikkhah, Karim, et al. “Efficacy and safety of Vicia faba L. extract compared with levodopa in management of Parkinson’s disease and an in-silico phytomedicine analysis.” International Journal of Ayurvedic Medicine 14.3 (2023): 794-800.
Rijntjes, Michel. “Knowing your beans in Parkinson’s disease: a critical assessment of current knowledge about different beans and their compounds in the treatment of Parkinson’s disease and in animal models.” Parkinson’s Disease 2019 (2019).
Vered, Y., et al. “Bioavailability of levodopa after consumption of Vicia faba seedlings by Parkinsonian patients and control subjects.” Clinical neuropharmacology 17.2 (1994): 138-146.
Morais, L. C. S. L., J. M. Barbosa-Filho, and R. N. Almeida. “Plants and bioactive compounds for the treatment of Parkinson’s disease.” Arquivos Brasileiros de Fitomedicina Científica 1 (2003): 127-132.
Shetty, Kalidas, Reena Randhir, and Dipayan Sarkar. “Bioprocessing strategies to enhance L-DOPA and phenolic bioactives in the fava bean (Vicia faba).” Functional Foods and Biotechnology. CRC Press, 2019. 99-114.
